
Pulled Muscle? Sprained Ankle? Sore Elbow?
“Ice it”
R.I.C.E, Right?
Rice: Rest, Ice, Compression, Elevation.
That’s been the go-to advice for, well, since I can remember.
Just watch any athletic event.
Baseball pitchers with their shoulders and arms completely encapsulated in ice.
NFL and NBA sidelines with feet up and ice packs plastic wrapped to ankles and knees.
We Do It This Way Because It’s Always Been Done This Way
Is usually the worst answer ever…
Yes, it might be effective.
But, is that practice OPTIMAL?
Shouldn’t the answer be,
We Do it This Way, Because We Have EVIDENCE That it Works and is BEST PRACTICE.
Me thinks so.
Hans Selye, Stress and Why Ice Aint Always Nice
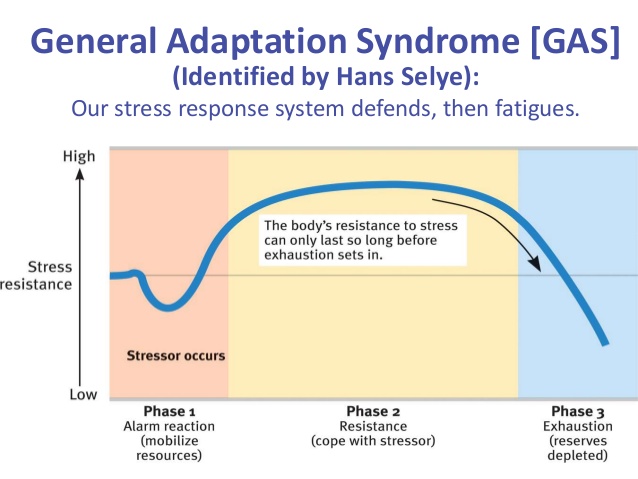
GAS: General Adaptation Syndrome:
“GAS is the three-stage process that describes the physiological changes the body goes through when under stress. Hans Selye, a medical doctor and researcher, came up with the theory of GAS. During an experiment with lab rats at McGill University in Montreal, he observed a series of physiological changes in the rats after they were exposed to stressful events.
With additional research, Selye concluded that these changes were not an isolated case, but rather the typical response to stress. Selye identified these stages as alarm, resistance, and exhaustion.” – Healthline
Pictures help us learn better:
 Whats Ice Got to Do With It?
Whats Ice Got to Do With It?
Ice is typically used immediately following a soft tissue injury.
The period, immediately following the injury (tissue deformation), that would correspond to Phase 1 of the GAS.
For example: let’s think of the blue line in the above graphic as the tissues of your ankle.
The dip = Once the body has “realized” you’ve sprained your ankle and mobilized adaptive resources.
I Have Met Him, and His Name is Inflammation:
inflammation seems like one bad hombre,
Is your food causing inflammation? – Dr. Oz.
Here, just take two of these to take the inflammation down. – Your Doc
“It’s the systemic inflammation.” – Dude you know who just read an article on the internet.
The last one, systemic inflammation, is my favorite, cause 9/10 times whoever says it has zero idea what that means.
This Bed’s Too Hard, This Bed’s Too Soft, This One is Juuuussssst Right
Like Most Things in Life;
Inflammation isn’t always a gad Guy,
“Inflammation isn’t Always Bad For You. Inflammation is the ONLY Reason You Adapt…PERIOD” – Dr. Andy Galpin
He’s just a dude, doing what he does.
But we need CONTEXT, an understanding of biology and the whole statement helps too:
“Inflammation isn’t Always Bad For You. Inflammation is the ONLY Reason You Adapt…PERIOD. But A Lot of Inflammation, All the Time, Is Really Bad For You” –Dr. Andy Galpin
See, inflammation kids, is the FIRST STEP IN THE RECOVERY PROCESS.
“Inflammation is one of the most important mechanisms of host defense since it marshals the attack on the injurious agent and leads to repair of the affected tissue” – The Role Of Inflammation in the Healing Process
Inflammation is what sends the signal to STOP/ control tissue breakdown and BEGIN REPAIR processes.
“Inflammation is the body’s mechanism for coping with agents that could damage it. In other words, inflammation is a protective response to rid the body of the cause of cell injury and the resultant necrotic cells that cell injury produces. Although the processes of acute and chronic inflammation are an important protective mechanism used by the body to deal with potentially damaging agents, they are potentially damaging to the body and must be closely regulated. The basic steps in acute inflammation allow white blood cells to move from the blood to the tissue location where they are required. Acute inflammation can resolve completely if the inciting agent is removed, or it can have one of several other sequelae, including chronic inflammation.” – Pathology: The Big Picture
An Inflammation Free Life is One in Which No Recovery Takes Place
So inflammation is NEEDED for the repair process to being and move the body through Stage 1 of the General Adaptation Syndrome (GAS) and into Stage 2 which would hopefully encompass recovery or supercompensation.
As I outlined here, in an article about minimal effective dose and maximal recoverable volume, most things in physiology, fit nicely into the inverted U (Yerkes- Dodson Hypothesis) .
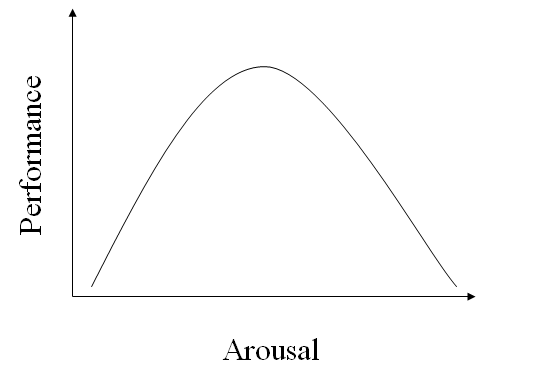 The Yerkes- Dodson was developed with psychological arousal and sport performance, but the theory holds true for most things in life.
The Yerkes- Dodson was developed with psychological arousal and sport performance, but the theory holds true for most things in life.
Summed up as such,
Not Enough is Not Enough, Some is Better, Optimal is Best, Too Much is Bad.
It’s when inflammation goes off the rails, its rampant, and you’re unable to resolve the injurious agent and therefore inflammation response to that agent (stressor) in a chronic/ systemic state, that inflammation is a bad thing.
“Chronic inflammation inevitably causes tissue damage and is accompanied by simultaneous attempts at healing and repair. The exact nature, extent and time course of chronic inflammation is variable and depends on the balance between the causative agent and the attempts of the body to remove it” – Dr. William Bennet
Without inflammation, we’re screwed, the body never marshals its adaptive reserves to supercompensate…..we never recover.
What’s Ice Got to Do With it?
The use of cryotherapy, applying ice to an injured tissue, may BLUNT the inflammation response.
“greater elevations in circulating CK-MB and myoglobin above the control level were noted in the cooling trial during 48-72 hours of the post-exercise recovery period. Subjective fatigue feeling was greater at 72 hours after topical cooling compared with controls. Removal of the cold pack also led to a protracted rebound in muscle hemoglobin concentration compared with controls. Measures of interleukin (IL)-8, IL-10, IL-1β, and muscle strength during recovery were not influenced by cooling. A peak shift in IL-12p70 was noted during recovery with topical cooling. These data suggest that topical cooling, a commonly used clinical intervention, seems to not improve but rather delay recovery from eccentric exercise-induced” muscle damage.” – Tseng, Lee and super friends
“The results demonstrate that cryotherapy can create a deep state of vasoconstriction in the local area of treatment. In the absence of independent stimulation, the condition of reduced blood flow persists long after cooling is stopped and local temperatures have rewarmed towards the normal range, indicating that the maintenance of vasoconstriction is not directly dependent on the continuing existence of a cold state. The depressed blood flow may dispose tissue to NFCI.”- Khoshnevis S1, Craik NK, Diller KR
“The hypothesis that prolonged cooling reduces posttraumatic microvascular dysfunction, inflammation, and structural impairment was confirmed.” – Schaser KD1, Disch AC, Stover JF, Lauffer A, Bail HJ, Mittlmeier T.
But other stuff you’d want to reduce happened here too, so maybe ice does have a place? <—-more to come.
Lets keep in mind, human biology is really cool.
But it ain’t fool-proof.
Not Everything that Happens “Naturally” is Best,
“The inflammation associated with fresh injuries is indeed mostly biology business as usual, a normal “side effect” of healing. But not all of it! Not everything “normal” in biology is wise and good and never needs to be controlled or treated.3 Diarrhea is natural, too. Inflammation can and does get out of hand, and we know that at least some of it is actually “bad” biology, naturally excessive, that does not benefit us in any way.4″- Pain Science, Icing For Injuries
What it really comes down to is NOT that ice is bad, or good, but instead this;
“The physiological effects of cold therapy include reductions in pain, blood flow, edema, inflammation, muscle spasm, and metabolic demand. There is limited evidence from randomized clinical trials (RCTs) supporting the use of cold therapy following acute musculoskeletal injury and delayed-onset muscle soreness (DOMS).” –Mechanisms and efficacy of heat and cold therapies for musculoskeletal injury.
So maybe icing acute injuries, something we’ve done forever, might not be the best, EVIDENCE BASED, practice?
“Despite its widespread clinical use, the precise physiologic responses to ice application have not been fully elucidated. Moreover, the rationales for its use at different stages of recovery are quite distinct. Using cryotherapy to manage acute soft tissue injury is based largely on anecdotal evidence.” – Journal of Athletic Training
When All You Have is A Hammer, Everything Looks Like A Nail
We should think critically about ice as a universal modality for every soft tissue injury, especially since there is little to no evidence to support it as a treatment and instead THINK about the situation at hand and ALL of the tools available to do the job.
If you read some of the effects of ice described above those seem to be really good things for treating an acute injury like:
- Limiting pain
- Excessive swelling
- Reducing structural impairment
- Did I mention, limiting pain?
Limiting Pain Is a BIG Reason to Use Ice
“Icing is primarily an analgesic — a pain-reliever — and not an actual treatment.” – Pain Science
Even Dr. Mirkin, the man who came up with R.I.C.E and later recanted it says,
“Since applying ice to an injury has been shown to reduce pain, it is acceptable to cool an injured part for short periods soon after the injury occurs. You could apply the ice for up to 10 minutes, remove it for 20 minutes, and repeat the 10 minute application once or twice. There is no reason to apply ice more than six hours after you have injured yourself”.- Dr. Mirkin
If ice makes the injury site feel better you’re probably going to be able to begin actual treatment modalities sooner.
And a large part of those effective treatment modalities is gently using/ moving the injured site,
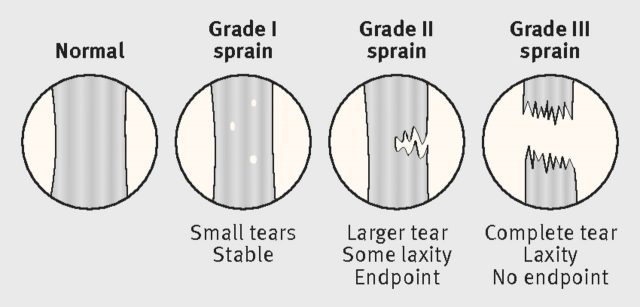
The NATA researchers found level “A” evidence supporting functional rehabilitation — in other words, therapies that involve moving the ankle soon after the injury — for ankle sprains of grade I (stretching and damage to ligament fibers) and grade II (partial tearing of the ligaments).
No one recommends forcing patients to walk on their sprained ankles right away. But some randomized controlled trials have shown that beginning range-of-motion exercises within a couple of days, followed by gradual loading, can get patients back on their feet more quickly.[6] Manipulation of the joint by trained therapists has also shown success in these trials.[6]
For grade III ankle sprains (complete ligament tear), Kaminski and colleagues found “B” level evidence for immobilizing the joint for 10 days.[6] After that, they recommend, patients should begin moving the joint. – Medscape Orthapedics
When is Ice Nice?
Here’s MY guideline.
I’m not a MD, DPT, PT or ATC, so there is that.
BUT, I have been trained in smashing weights, being awesome and dominating life. <—-and have jacked myself up in every conceivable way possible, multiple times.
So there’s that too.
This is simply what has worked FOR ME and the IMMEDIATE advice I would give someone.
Low grade Sprain or Strain:
Do you LIKE ice?
Yes?
Use it.
No?
Skip it.
Either way, you’re probably not helping or hurting the tissue long-term.
Pull your neck when you get up in the morning?
Tweak your low back squatting?
Ice Isn’t Going to Help, it’s Probably Going to Prolong the Injury.
The tissue damage is really limited, no tissues are unstable, the tissues are just “disorganized”.
The body isn’t going to go crazy with inflammation, it’s just going to be a tight, stiff, sore, pain in the ass, for the rest of the next couple days.
Cryotherapy (ice) will only stiffen up the already tight tissues and slow the healing process that, if left alone, or possibly accelerated through heat therapy (more on that next week) would be good to go in a day or two.
For a “Real” Injury?
One where tissue is/ could very likely be torn.
Typically this is going to be a Grade 2 or 3 sprain or strain.
 From this article: Management of Ankle Injuries
From this article: Management of Ankle Injuries
The kind with immediate swelling, bruising, mobility limitations, moderate to severe pain, stuff that you’re going to be seeing a medical professional ASAP?
Ice that Bit#h.
Apply the tool where and how it works best.
Control the swelling, edema, peripheral tissue death and control the pain.
Go see the doc or your PT and get it right.
Before we move on to next week and the case for heat:
A Not So Quick Note on Professional Boundaries and “Scope of Practice”:
This is a real grey/ gray area for me and any trainer. when it comes to injuries and treatment.
Lets think about it this way:
IF a low-grade injury, the typical sprain or strain happens in the gym, under my watch, wouldn’t I be the MOST PROXIMAL “Professional” with training in the care and treatment of that injury and have a PROFESSIONAL RESPONSIBILITY to activate immediate care?
There are those who think we, as trainers, should give no advice and let our clients:
- Do whatever they please following an injury
- Go home
- Make an appointment with the GP and maybe get a referral for Physical Therapy
- Wait to get in to see the therapist…
And waste 2 days-3 weeks of basic care and rehabilitation, ya know, doing stuff to get better, cause you had a sore elbow after benching and I’m not a Physical Therapist or MD?
Plus, I think the CONTEXT is important here.
I’m talking about dealing with your immediate or even the little “nagging” sports injuries.
Applying ice or heat so you can function at 95%, instead of 80%, not your surgical options.
These are Acute, Low Level, Injuries.
The kind where the MD goes,
“take some ibuprofen and rest it for 2 weeks.”
Where, you’re not injured, you’re hurt and the reality is;
If it was a playoff game, you’d play.
But the coach is gonna let ya “take a veterans day” and sit out practice to “get some rest” during the preseason, type of thing.
If we ran off to the doctor’s office or physical therapist every time we had an ouchie, a bump, bruise, strain or sprain,
We’d Spend All Our Days In A Medical Office
 I’m not trying to replace your Orthopedist or Physical Therapist, if they evaluate an injury and tell you to do something, DO IT.
I’m not trying to replace your Orthopedist or Physical Therapist, if they evaluate an injury and tell you to do something, DO IT.
“Physical therapists and orthopedic specialists work specifically to fix what is broken or severely injured, whereas personal trainers and coaches work to enhance what is not broken. Put simply, training consists of assessing what they currently have and using general exercise to improve on what they currently have while working around what is broken or severely injured.” – The Scope of Practice for Personal Trainers
I think its logical that little bit of tissue deformation (slight injury) isn’t “broken or severely injured”.
I mean, from a physiological perspective, is DOMS (delayed onset muscle soreness) and a low-grade sprain or strain physiologically any different?
If the injury/ pain/ impairment is having an impact on your quality of life….You’re broken or severely injured.
GET SOME QUALIFIED MEDICAL ATTENTION.
What the aim of these articles is, is to give you an understanding of what might be the best treatment for the sore knee or cranky back you have after working out today because:
- You were (hopefully) going to treat it yourself anyway <—-which has almost always meant icing and that might not be best for THAT situation
- You had NO PLANS on making an appointment, going to an office, paying the copay or deducible and seeking medical advice right now cause aint no body got time fo’ dat.
- Doing something that may accelerate the healing process and cut the ouchie down from 3 days of pain to one is something worth doing.
Again, actue, low-grade, injuries.


Roy, you’ve done it again. Thanks for your evidence(!)-based approach.
I try….thanks for reading, and the comments…You’re the best.